Prevention of nosocomial infections (hospital infection) in medical facilities (in Japanese only)
Prevention of nosocomial infections at medical institutions (in Japanese only)
Basic Knowledge of Infection
Establishment of Infection
Infection is said to occur when a microbe enters an organism and settles and multiplies in the organism and becomes a parasite. Three elements (the three elements of infection) are required for infection to occur.
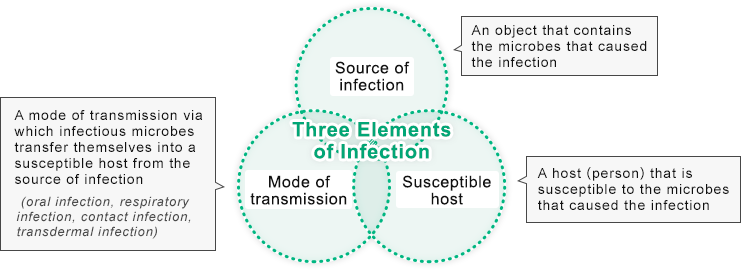
The mechanism of these three elements is referred to as the "chain of infection," and the principle of infection control is to break this chain. The U.S. Centers for Disease Control and Prevention (CDC) provides specific measures for infection control as per the following categories.
2. Transmission-based precautions
3. Occupational infection prevention and control
Infection Control
Microbes that cause infection are extremely small groups of organisms—so small that they are usually invisible to the naked eye and can only be observed under a microscope. Some diseases caused by these microbes were once referred to as the "plague" and have caused human suffering for a long period of time. In some respects, the history of medicine can be said to be the history of the battle against these microbes.
Standard Precautions
In 1996, the CDC published a set of precautions, called "Standard Precautions." It recommends that all patients, regardless of whether they are infected or not, take the following measures to reduce the risk of transmission of microbes via blood, body fluids, secretions, excretions, wounds, and mucous membranes.
2. Gloves
3. Masks/goggles
4. Gowns
5. Devices
6. Linen
Transmission-based Precautions
To prevent nosocomial infections, the main focus is to block the routes of infection. The routes of nosocomial infection include people, objects, and air.
| People | Hair | Wearing caps |
|---|---|---|
| Respiratory droplets | Wearing a mask | |
| Hands and fingers | Washing hands and wearing gloves | |
| Clothing | Control and sterilization of clothes | |
| Covering materials | Dust control | |
| Objects | Devices to be used | Must be sterilized (aseptic processing), use of disposable products |
| Air | Aseptic room via a HEPA filter | |
Nosocomial Infections
In general, the following factors are considered to be nosocomial infections.
1. Increase in the number of patients with weaker resistance to infection
2. Patients with serious underlying diseases, premature infants, newborns, the elderly, etc.
3. Treatments and examinations that reduce a patient's resistance
4. Immunosuppressive drugs, anti-cancer drugs, catheters, major surgery, chemotherapeutic drugs
5. Disruption of normal defense functions
6. Shunts and tracheotomy for surgery, catheterization, and dialysis
7. Chemotherapeutic drugs, long-term use of third-generation antibiotics, etc.
8. Increase in multi-drug-resistant bacteria, increase in opportunistic pathogens
9. Problems of structure in hospital rooms and room sharing, pollution within a hospital
10. Problems with visitors from the outside and medical-related items
11. Choosing incorrect disinfectants or sterilization methods, etc.
Explanations of the concept of infectious diseases and countermeasures are available on the website of Japan's Ministry of Health, Labour and Welfare.
Basic concept of the "prevention of nosocomial Infection (hospital infection) in medical facilities"
Basic concept of "infection control for COVID-19"
Surgical Site Infections (SSIs)
"SSI" refers to wound infection, intraperitoneal infection, and intraperitoneal abscess. All of these are infections that occur within 30 days after surgery (or within a year if there is an implant). SSIs do not include retrograde infections from draining or distant part infections such as respiratory or urinary tract infections.
Background and Current Situation in the U.S.
SSIs came to attract attention because of the following reasons.
1. Importance of preventing SSIs during high-risk surgical procedures, not just in terms of skin and subcutaneous
tissue infections
2. Changes in the awareness of health care professionals and patients regarding infection during medical procedures
3. Issuance of CDC guidelines for the prevention of SSIs in 1999
In the U.S., the CDC Hospital National Nosocomial Infection Surveillance (NNIS) surveillance system has been collecting data for more than 20 years, and huge amounts of data have been sent to hospitals as feedback regarding infection control indicators. According to some of the NNIS's publications, approximately 14‒16% of inpatients in the U.S. are experiencing SSIs, with two-thirds of the infections occurring only in surgical wounds and the remaining one-third of infections occurring in or around the organs where the surgery was performed. It is reported that 77% of deaths among patients with SSIs are directly attributable to SSIs.
Precautions
In order to reduce surgical site infections, the CDC has analyzed risk factors in the surgical field and preventive measures based on clinical data from the following perspectives. In Japan, Chapter 7 of the Practical Guideline for Surgical Treatment provides specific items to prevent SSIs, and many medical institutions are making efforts to prevent the occurrence of SSIs, because once such occurs, the hospital stay is prolonged, medical costs increase, and as a result, patients satisfaction with surgical treatment decreases.
- Use and choice of antimicrobial agents to prevent post-operative infections
- Management of patient complications
- Disinfection and environmental management of operating rooms
- Disinfection and infection control for medical professionals
HOGY Medical handles a variety of products that contribute to the prevention of SSI outbreaks from two aspects: improvement of medical quality (provision of high-quality medical care) and the hospital management of medical institutions.

